ILD-related comorbidities
A comorbidity is a disease or condition that is associated with the primary disease. Comorbidities are associated with worse health outcomes, more complicated management, and worse quality of life. Early identification and treatment of comorbidities associated with ILD are very important for keeping you as healthy as possible. Many of the questions your provider asks you during your initial visit have to do not only with diagnosing your ILD but also with looking for possible comorbidities.
Here are some common comorbidities associated with ILD:
GERD

Gastroesophageal reflux disease (GERD), also known as acid reflux, occurs when stomach contents back up — or reflux — into the esophagus. This can be due to weakening of the muscle where the esophagus meets the stomach, called the lower esophageal sphincter, or to problems with the contractions of the esophagus or stomach.
Many studies have shown a link between GERD and lung disease, including ILD. The reason for this relationship is unclear. One theory suggests that reflux may play a role in the development of certain lung diseases. The link between ILD and GERD is an active area of research in the UCSF ILD Program.
Signs & Symptoms
Common signs and symptoms of GERD include:
- Heartburn (burning sensation in the center of the chest)
- Regurgitation of food and liquid
- Acid or sour taste in the throat
- Chest pain
- Cough
Less common symptoms include stomach pain, sore throat, hoarse voice, difficult or painful swallowing, recurrent pneumonia, asthma, chronic sinus infection or a sensation of a lump in the throat.
Diagnosis
In the general population, doctors can often diagnose GERD by taking a medical history and performing a physical examination. In patients with ILD, diagnosis is more complicated, as patients may have unusual symptoms or may lack symptoms. In ILD patients, additional testing is often needed to diagnose GERD.
In addition to taking a medical history and performing a physical exam, your doctor may recommend the following tests:
- Esophageal pH monitoring — This is the most direct way to measure the frequency of acid reflux. The test involves inserting a thin tube into the nose and down into the esophagus. The tube is left in for 24 hours while it measures how much stomach acid is getting into the esophagus.
- You can eat and drink normally during this test. Most patients have very few side effects from the test, the most common being a sore throat. Once the test is complete, you'll need to return to have the tube removed.
- Esophageal Manometry — By measuring the muscle contractions of your esophagus, this test can tell your doctor if your lower esophageal sphincter is functioning properly. The test is often done at the same time as the initial placement of the 24-hour pH monitor.
- Upper GI Series — Also called a barium swallow, this test can help your doctor determine if you have a swallowing problem that may mimic signs and symptoms of GERD. The test involves swallowing barium, a contrast material that shows up on X-rays, while a technician takes an X-ray series of your chest and neck.
- Endoscopy — This procedure allows us to see your esophagus with an endoscope, a camera mounted on a small, flexible tube. Endoscopy is performed by a gastroenterologist and is an outpatient procedure. The test reveals if there's any damage to the lining of the esophagus from chronic acid exposure.
Your doctor may recommend an endoscopy if you're experiencing painful swallowing, unexplained weight loss or bleeding (dark-colored stools or vomiting blood).
Treatment
The treatment for GERD depends on the severity of the disease. All patients should make changes to their diet and lifestyle to reduce the symptoms and complications of GERD.
It's important for patients to realize that we don't know if treating GERD influences the course of the underlying lung disease. However, patients should discuss treatment with their doctors, in order to avoid the long-term complications of uncontrolled GERD.
Lifestyle Changes
Lifestyle changes include:
- Weight loss
- Smoking cessation
- Raising the head of your bed 6 to 8 inches — you can use either blocks of wood under the legs of your bed, or a foam wedge under your mattress
- Avoiding foods that cause acid reflux: caffeine, chocolate, alcohol, peppermint, and fatty or spicy foods
- Avoiding large and late meals — don't lay down immediately after eating, and eat three or more hours before bedtime
Medications
Medications for mild GERD include:
- Antacids — These provide short-term relief. Examples include Tums, Maalox and Mylanta.
- Histamine antagonists — These reduce acid production in the stomach, but are less effective than proton pump inhibitors, described below. Examples include ranitidine (Zantac), famotidine (Pepcid) and cimetidine (Tagamet).
Medications for moderate to severe GERD:
- Proton pump inhibitors (PPI) — PPIs reduce acid production in the stomach. Examples include omeprazole (Prilosec), esopmeprazole (Nexium), lansoprazole (Prevacid), dexlansoprazole (Kapidex), pantoprazole (Protonix) and rabeprazole (Aciphex).
These medications are generally safe and well tolerated, but if taken for long periods of time they may increase the risk of pneumonia, gut infections or bone fractures.
If these treatments don't control your symptoms, your doctor may consider a different PPI or increase the dose of your PPI. In the most severe circumstances, your doctor may recommend surgical treatment for your GERD.
See www.aboutgerd.org for more information.
Pulmonary Hypertension
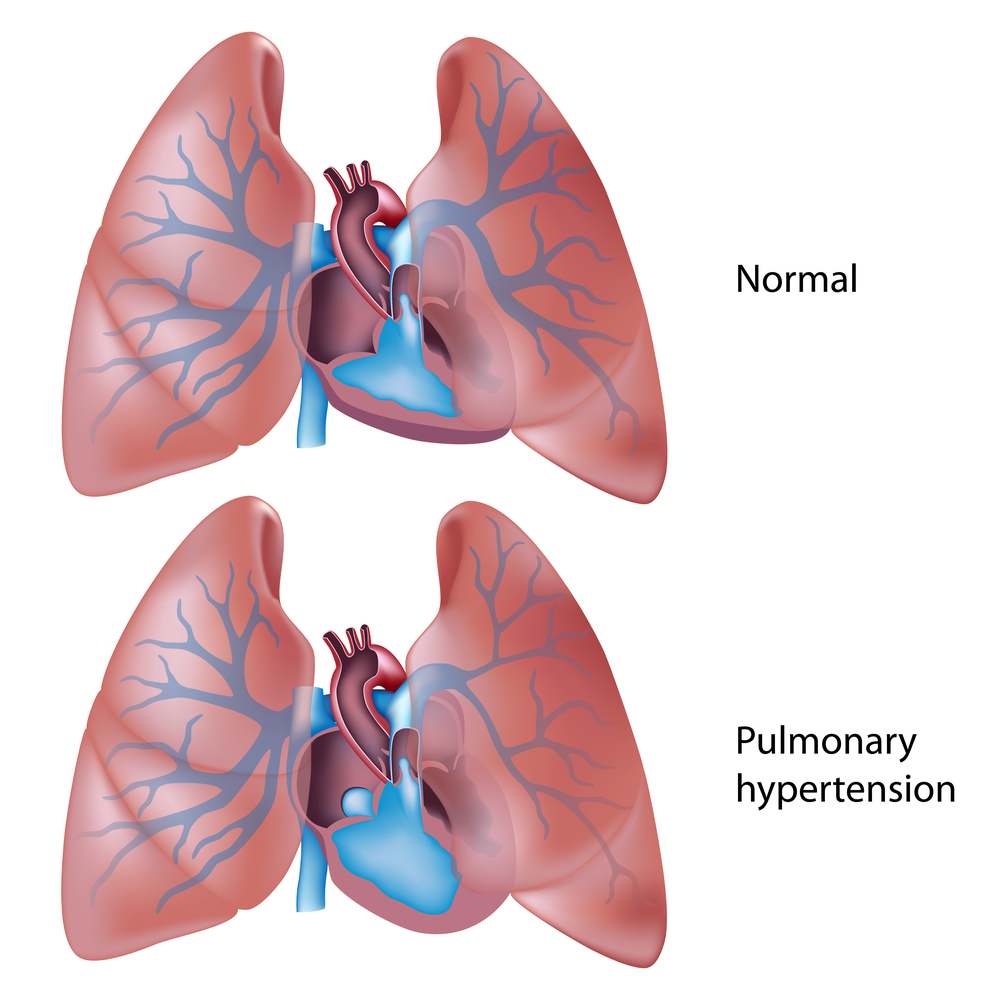
Pulmonary hypertension (PH) is a blood vessel disorder of the lungs. It can be associated with diseases of the lungs, including interstitial lung disease. In pulmonary hypertension, the walls of the blood vessels in the lungs become stiff and thick and inflamed. This can reduce or block the flow of blood through the blood vessels and cause high blood pressure in the lungs. Pulmonary hypertension should not be confused with regular high blood pressure or hypertension. Pulmonary hypertension can occur in people with or without regular hypertension.
Signs and Symptoms
Symptoms of PH are similar to those of ILD. Patients with PH often complain of shortness of breath with physical activity that gradually worsens over time.
Patients may also experience the following symptoms:
- Chest pain
- Fainting episodes
- Difficulty breathing when lying flat
- Swelling of the ankles
In ILD patients, pulmonary hypertension is usually suspected when these symptoms are out of proportion to the severity of the patient's ILD.
Diagnosis
In diagnosing PH, your doctor will start by conducting a thorough medical history and physical examination. This will include discussing your other medical problems, which may be associated with PH. A review of your medications and exposures is important, since certain diet pills and recreational drugs can increase the likelihood of having PH. The physical exam, which includes listening to your heart sounds and observing your neck veins, may also reveal findings suggestive of PH.
Your doctor may also conduct the following tests to make an accurate diagnosis:
- Echocardiogram — This is an ultrasound study that provides your doctor with video images of your heart and how it is functioning. We can estimate the blood pressure within your lungs based on the speed at which blood flows through your heart.
- Blood Tests — Certain blood tests, specifically for a polypeptide called B-type natriuretic peptide (BNP), can help support the diagnosis of PH. BNP is released into the blood when the heart is under strain, which often occurs as a result of PH.
- Right Heart Catheterization — This procedure is required to definitively diagnose PH. A short catheter (a thin, flexible tube) is placed into your neck or groin, and then a smaller, longer catheter is guided through it. This technique is used to directly measure the blood pressure in your lungs.
- Computed Tomography (CT) Angiogram — In patients with documented PH, CT angiography may be performed to look for potential causes. This is a special type of CT scan used to study the blood vessels in your lungs. For the blood vessels to appear on the scan, contrast dye will need to be injected into a vein in your arm at the time of the CT.
- Ventilation-Perfusion Scan (V/Q scan) — In patients with documented PH, V/Q scanning may be performed to look for potential causes. A very small amount of radioactive tracer is injected and inhaled to determine whether blood is flowing appropriately to those areas of the lung that are receiving oxygen.
Treatment
Treatment for PH can be divided into two main categories: supportive therapy and PH-specific therapy. Supportive therapy is used to treat the underlying factors which may worsen PH, and to prevent complications. PH-specific therapies are designed to reduce the blood pressure within the lungs.
Several PH-specific therapies have recently been approved by the U.S. Food and Drug Administration (FDA) for use in patients with other forms of PH — specifically pulmonary arterial hypertension. The efficacy of these therapies in patients with PH and ILD remains uncertain. Using PH-specific therapy in ILD patients remains controversial, so you should discuss the benefits and risks with your provider.
Supportive therapy
- Oxygen — Supplemental oxygen helps increase oxygen supply to the blood and helps prevent narrowing of the pulmonary blood vessels, which can worsen PH.
- Diuretics — Diuretics, or water pills, help prevent swelling and are sometimes useful in improving heart and lung function in PH patients.
- Anticoagulants (blood thinners) — Anticoagulants are sometimes required if blood clots are detected in the lungs or if PH is severe.
- Pulmonary Rehabilitation — Pulmonary rehabilitation has been shown to improve outcomes in patients with ILD, as well as patients with PH. Be sure to tell your pulmonary rehabilitation provider if you have been diagnosed with PH.
PH-specific therapy
- Prostanoids (Flolan, Treprostinil, Iloprost) — Prostanoid, or prostacyclin, therapy is available as a continuous intravenous infusion or as an inhaled medication. Prostanoids are rarely used for PH in patients with ILD.
- Endothelin Receptor Antagonists (Bosentan, Ambrisentan) — Endothelin receptor antagonists are taken by mouth. Patients who take them must have their liver function monitored regularly.
- Phosphodiesterase Inhibitors (Sildenafil) — Phosphodiesterase inhibitors are taken by mouth. They should not be used in patients taking nitrates (for example, nitroglycerin) for heart disease.
Prognosis
Survival in patients with ILD and PH is worse than in ILD patients without PH. Several research studies are now looking at the role of PH treatment in improving the prognosis for these patients. If you are a good candidate for a lung transplant and have progressively worsening ILD and PH, your doctor may refer you to a specialist for a lung transplant evaluation
Obstructive Sleep Apnea
Obstructive sleep apnea (OSA) is a potentially serious sleep disorder that causes breathing to repeatedly stop and start during sleep, therefore decreasing oxygen saturation of the blood. This happens because, during sleep, the tongue and soft palate fall back against the back of the throat, blocking off the airway. Every time the airway becomes blocked, the person stops breathing and wakes up. This can happen hundreds of times a night, and often for a minute or longer. Sleep, then, is constantly interrupted and of very poor quality, and oxygen saturation of the blood is low. The person may not be aware that this is happening - only, perhaps, that they are sleepy during the day.
Risk Factors
Risk factors for OSA include older age, obesity, male gender, post-menopausal women, large neck circumference, recessed chin, smoking and alcohol use, family history of sleep apnea, asthma, chronic nasal congestion. OSA is also common in people with fibrotic lung disease.
Signs and Symptoms
Signs and symptoms of OSA include excessive daytime sleepiness, loud snoring, observed episodes of breathing cessation during the night, abrupt awakenings due to gasping or choking, awakening with a dry mouth or sore throat, morning headache, memory problems, difficulty concentrating, depression, GERD.
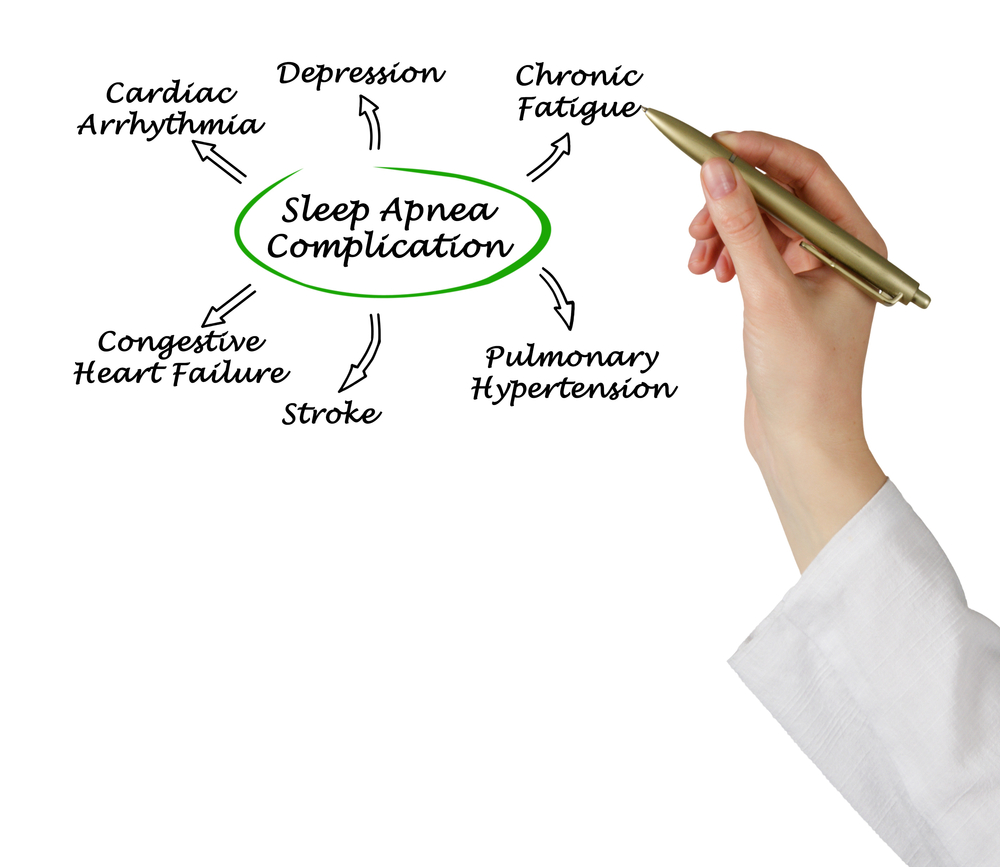
Complications
Untreated sleep apnea can lead to high blood pressure and heart problems, stroke, diabetes, weight gain, complications with medications and surgery, and falling asleep inappropriately, such as during driving.
Diagnosis
The diagnosis of sleep apnea is done by a pulmonologist with a specialty in sleep - a sleep specialist. S/he will talk to you about your history, perform a physical examination, other tests as needed, and order polysomnography, also known as a sleep study. You may either go to a sleep lab for this, or your provider may give you an at-home version of the sleep study.
During an overnight sleep study, the heart, lung and brain activity, breathing patterns, snoring, arm and leg movements, blood oxygen levels are monitored. Sometimes the monitoring is performed all night, and sometimes, in a “split-night sleep study”, this monitoring occurs during the first half of the night, and then, if you’re diagnosed with OSA, the staff will wake you up and administer and adjust continuous positive airway pressure (CPAP) for the rest of the night.
Treatment
Treatment for OSA includes lifestyle changes:
- Weight loss for those who are overweight
- Regular exercise
- Decrease or avoidance of alcohol, sleeping pills and tranquilizers
- Quitting smoking
- Side sleeping - no sleeping on the back
- Oral appliances worn at night that prevent airway obstruction by re-positioning the lower jaw
- Continuous positive airway pressure (CPAP) - This is the most common treatment for OSA. Air is blown into the lungs using an air compressor and small mask or nasal pillows. The air pressure keeps the airways from being blocked. To be effective, CPAP must be used whenever sleeping. CPA is a very effective treatment for OSA. Unfortunately, some people can’t tolerate CPAP - the mask is uncomfortable, they feel claustrophobic or anxious, etc.
- Surgery - Surgery is usually considered second-line therapy for OSA. Surgery is tailored to the specific area of obstruction in a particular patient - nose, soft palate, tongue, lower jaw, or a combination of these.
For additional information American Sleep Apnea Association's website has more in-depth information, education videos, and podcasts around the subject that you may find very helpful.